Addressing the “access” and “scale” challenge: effectiveness of a new WHO guided psychosocial self-help programme

Project overview
To help improve the evidence base and availability of psychosocial interventions that are scalable and accessible even when humanitarian access is limited
Countries
Uganda
Organisations
World Health Organisation
Partners
Peter C Alderman Foundation (PCAF), Makerere University, Johns Hopkins University, Institute of Psychiatry, Kings College London, University of New South Wales, United Nations High Commissioner for Refugees (UNHCR), University of Ottawa, University of Glasgow
Area of funding
Humanitarian Research
Grant amount
£456,713
Start date
01
October
2015
End date
01
April
2018
Project length (in months)
30
Funding calls
Topics
No items found.
Status
Closed
Project solution
This project offers [specific solution or intervention] to tackle [challenge]. By implementing [strategies, tools, or innovations], the project aims to achieve [desired outcomes]. The approach is designed to [specific actions or methods] to bring about meaningful change in [community, region, or issue area].
Expected outcomes
This project aims to achieve [specific outcomes], such as [measurable results, improvements, or changes]. The expected impact includes [benefits to the target community, advancements in research or innovation, or long-term effects]. By the end of the project, we anticipate [specific changes or milestones] that will contribute to [broader goals or objectives].
Principal Investigator: Mark Van Ommeren, World Health Organisation
What did this study set out to achieve?
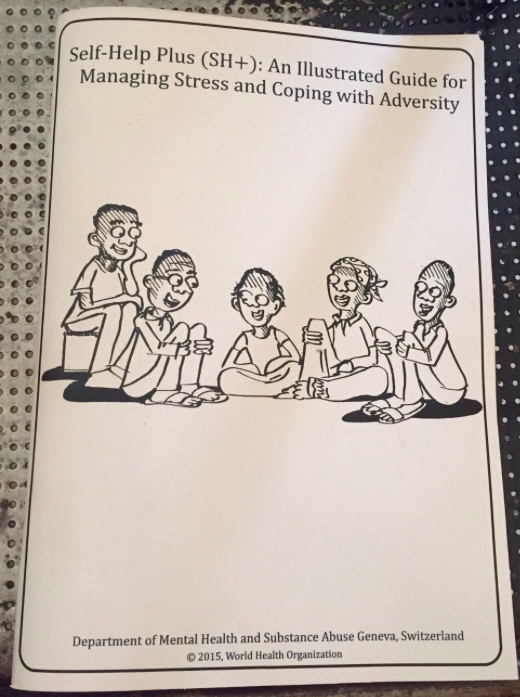
The overall objective of this research was to help improve the evidence base and availability of psychosocial interventions that are scalable and accessible even when humanitarian access is limited, thus overcoming current barriers to implementation of evidence-based support. The study aimed to evaluate the effectiveness of Self Help Plus (SH+) with South Sudanese refugee women. SH+ is an innovative WHO intervention package that;
- (a) is delivered to affected people via a 5-session guided self-help multimedia course;
- (b) ensures fidelity to evidence-based techniques via pre-recorded audio visual content and illustration-based self-help book;
- (c) can be implemented in areas where humanitarian access is limited; and
- (d) is likely readily scalable.
SH+ is based on acceptance and commitment therapy (ACT), a form of cognitive-behavioural therapy, with distinct features.
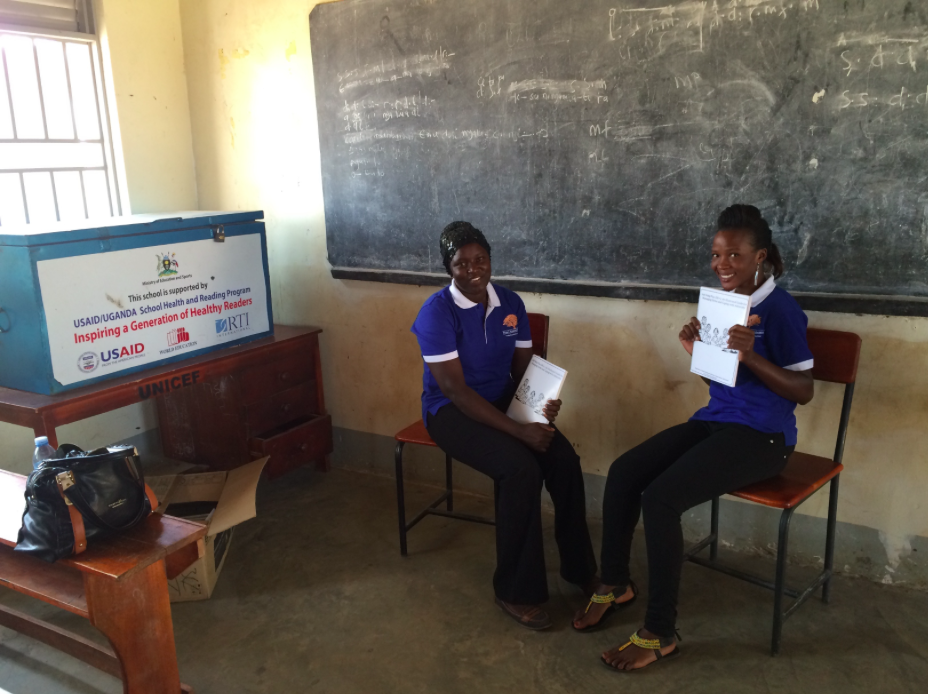
The research was successfully undertaken. A cluster randomised controlled trial was conducted among female South Sudanese refugees living in Rhino Camp Refugee Settlement in Northern Uganda. Fourteen villages were included in the definitive cRCT with 694 participants randomised to each condition. Baseline assessment included outcome measures of psychological distress, functional impairment, depression and PTSD symptoms, feelings of anger, interethnic relations, subjective wellbeing, psychological flexibility, as well as moderators (trauma history, adherence, health service use) and cost-benefit indicators. SH+ was provided by trained lay facilitators who had 12-16 years of education (e.g. post-secondary school diploma) but no previous clinical training or experience in providing mental health care. The primary outcome –levels of psychological distress– was measured immediately after SH+ and after 3 months with the Kessler 6 (K6) Scale.
What were the key findings?
- SH+ was shown to be effective and feasible to provide with minimal support / supervision.
- Among female adult South Sudanese refugees living in a refugee settlement in Northern Uganda, with moderate levels and above of psychological distress, delivery of the SH+ intervention compared with enhanced usual care resulted in clinically significant reductions in general psychological distress as well as secondary outcomes (e.g. functioning, wellbeing) at 3 months.
- The project also demonstrated the feasibility of delivering SH+ by an NGO suggesting that it can be implemented within existing health and community services. For example, SH+ could be provided at local health centres by community health workers or similar personnel.
- The study noted a high rate of engagement (83% average across all sessions) which suggests that SH+ might be attractive and meaningful to participants.
What does this mean for policymakers and practitioners?
Final adaptations were made to the SH+ package for South Sudanese populations (available on request from WHO – [email protected]) and SH+ is now included on the MHIN innovations website .
A second trial was funded by R2HC to ensure the results can be replicated with another population in another humanitarian setting. In addition, SH+ was tested in a trial with refugees in six European countries to look at its effects in preventing onset of mental disorder (funded by European Commission Horizons 2020 programme). On the basis of positive results from this research, WHO has now disseminated and published SH+ in 30 languages and as a web app, and has generated new research and innovation on its utility as a guided self-help intervention, including a completed RCT focused on health care workers in crisis settings. SH+ is now being implemented as part of the ongoing Ukrainian response across health, social protection, defence, education and security sectors, and in an increasing number of settings including in Türkiye as well as Uganda.
Dissemination of SH+ is also ongoing in Uganda and South Sudan including implementation research to further understand performance at scale. Elrha's Humanitarian Innovation Fund has funded SH+ under it's Journey to Scale programme, more information is available on the project page.
No items found.
Project delivery & updates
Stay up to date with the latest developments from this project. Here, you will find details on what has been delivered, resources created, and regular updates as the project progresses. Access key documents, reports, and other materials to see how the project is making an impact.
No resources/updates have been published yet for this project. Sign up for our newsletter to stay informed about upcoming publications and updates!
Join our Newsletter
Resources
No items found.
Latest updates
No items found.