Follow-up of Severely Malnourished Children (FUSAM): Effectiveness of a Combined Nutrition Psychosocial Intervention on Health and Development

Project overview
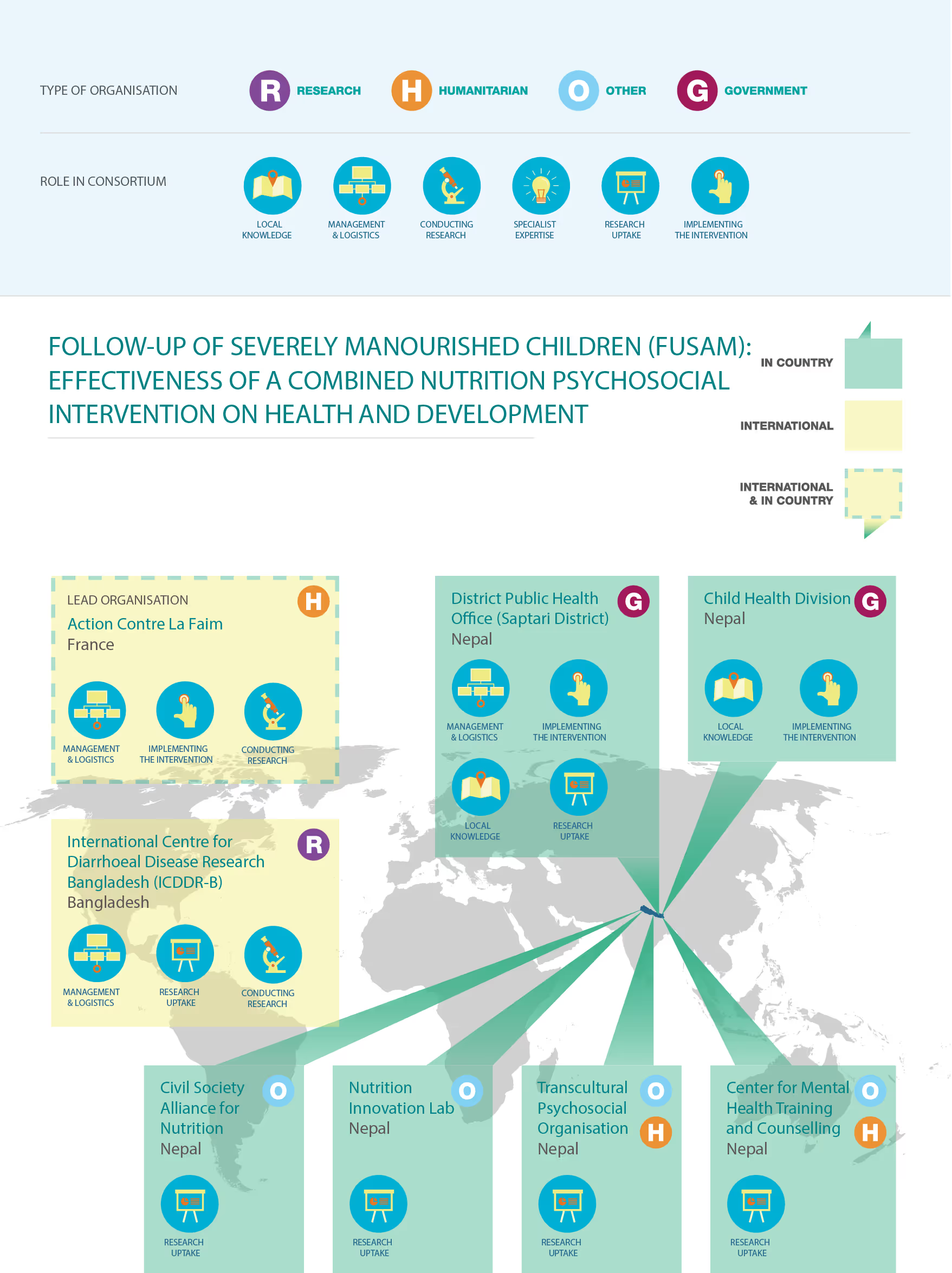
Funded by the R2HC in 2015, ACF's research intended to assess the cost-effectiveness and long-term impact of a brief combined nutrition/psychosocial intervention (in comparison to a stand-alone nutritional treatment) on the growth and development of children with SAM aged 6 to 24 months in the Saptari District of Nepal.
Project solution
This project offers [specific solution or intervention] to tackle [challenge]. By implementing [strategies, tools, or innovations], the project aims to achieve [desired outcomes]. The approach is designed to [specific actions or methods] to bring about meaningful change in [community, region, or issue area].
Expected outcomes
This project aims to achieve [specific outcomes], such as [measurable results, improvements, or changes]. The expected impact includes [benefits to the target community, advancements in research or innovation, or long-term effects]. By the end of the project, we anticipate [specific changes or milestones] that will contribute to [broader goals or objectives].
Principal Investigator: Cécile Bizouerne, Action Contre La Faim
Purpose
The study aimed to assess the cost-effectiveness and long-term impact of a combined nutrition/psychosocial intervention on the growth and development of children with Severe Acute Malnutrition (SAM) in the Saptari District of Nepal. The psychosocial intervention was aimed at mothers of malnourished children, and focused on empowering her as the key ally in the treatment of the undernourished child through improving child care practices, parent-child relationships and maternal mental health. The study planned to measure the impact on children’s nutritional outcomes, as well as child development and the mothers’ own mental health. A cost effectiveness study sought to investigate if the inclusion of the psychosocial intervention reduced overall treatment costs.
Outcomes
A randomised controlled trial was successfully undertaken and 640 children and their mothers were enrolled in the trial, including 427 children affected with SAM and 213 healthy children, aged 6 to 24 months. Data was collected at baseline, post-intervention and at 5 and 11 months after admission for children and caregivers who had received the intervention and those who had not, as well as a comparison group of children who were not suffering from SAM. The psychosocial programme involved 5 bi-monthly sessions linked to fortnightly visits to health centres for Outpatient Therapeutic Programme treatment. The psychosocial intervention involved sessions on communication and play; breastfeeding and feeding practices; massage, bathing, sleep and relaxation needs; and family sharing.
Key findings:
- Due to the substandard treatment protocol applied in Nepal, and the lack of completeness of the data on nutrition outcomes, the study could not confirm that the inclusion of a psychosocial support intervention had the anticipated effect on nutritional outcomes for children suffering from Severe Acute Malnutrition (SAM).
- Adding a brief psychosocial support within existing health services is possible in remote rural areas to promote positive parenting and enhanced child development. However, a brief intervention is not enough to compensate the difference in children development’s outcomes between those with and without SAM.
- The intervention showed promising impacts for the mothers’ own mental health. Mothers of children suffering from SAM demonstrated higher scores for depressive symptoms than children not suffering from SAM, indicating that programming targeting maternal mental health for caregivers of SAM children should be promoted.
- The planned cost effectiveness study was not able to draw conclusions as the effectiveness of the added psychosocial intervention could not be demonstrated. However a modelling study was undertaken which will inform optimal design of the psychosocial intervention.
Key outputs:
- Four articles are expected to be published, focusing on: effectiveness of psychosocial interventions on nutrition outcomes; maternal health and child development; mother-child interactions; and modelling effectiveness for nutrition sensitive interventions.
- An International Conference on Child’s Health and Development, addressing the challenges in linking children’s health and early childhood development, was held in Kathmandu in June 2017.
- A FUSAM psychosocial protocol manual will be developed and made available.
- A FUSAM study brief has been produced.
- An article has been published in Humanitarian Exchange on the implementation of the intervention.
Project delivery & updates
Stay up to date with the latest developments from this project. Here, you will find details on what has been delivered, resources created, and regular updates as the project progresses. Access key documents, reports, and other materials to see how the project is making an impact.
Resources
Journal article
LEARN MORE