Our planet, our health: three research studies to inform a changing climate

“The climate crisis is also a health crisis.” — Dr Ahmed Al-Mandhari, WHO’s Regional Director for the Eastern Mediterranean
There is no doubt that the largest global challenge facing us today is climate change. The recently published report by the UN’s Intergovernmental Panel on Climate Change (IPCC) warns that it is now or never to tackle the climate crisis. Human activities are altering our environment, whether we live in urban or rural areas, and our planet is becoming increasingly uninhabitable. Immediate action is needed to slow down the effect that climate change is having, and to better respond to the disasters and crises resulting from it.
The climate crisis also has direct consequences for our health. The World Health Organisation (WHO) has estimated that 13 million deaths a year are due to avoidable environmental causes. Rising temperatures, worsening air quality, deforestation and extreme weather events are disproportionally affecting people in low- and middle-income countries and in humanitarian settings.
Our Research for Health in Humanitarian Crises (R2HC) programme funds research in different crisis settings, aiming to strengthen the public health evidence base and inform humanitarian health response. The studies we fund seek to identify the most effective interventions to improve the health outcomes of people affected by crises.
Covering a broad range of global health issues, our research portfolio includes studies addressing health outcomes related to climate change, aiming to find ways to prevent and reduce its negative impacts on people’s health in humanitarian settings.
To mark World Health Day 2022 and its theme ‘Our planet, our health’, we thought we’d share three R2HC research studies which investigate health interventions related to the impact of climate change.

HEAT: Addressing illnesses caused by rising temperatures
‘HEAT (Heat Emergency Awareness and Treatment Bundle) Trial’. Study team: Johns Hopkins University School of Medicine, Aga Khan University, and Aman Foundation
Increases in global temperatures are causing a rise in heat-related illnesses. This is having a disproportionate impact on low- and middle-income countries. Interventions are needed to raise awareness about the linkages between extreme heat and health, and to mitigate the effect that global warming has on people living in some low-income settings.
Karachi, Pakistan’s most populated city, faced a huge tragedy in 2015. An extreme heat event caused the deaths of over 2000 people. The fragile health system was not able to cope, and healthcare professionals were not equipped with enough knowledge to recognise and treat heat stroke or other severe heat-related illnesses.
Observing the need for better preparation, this R2HC-funded study explored whether the Heat Emergency Education and Training (HEAT) training programme could better equip the city to deal with severe heat events in the future.
A training protocol for recognising and dealing with health impacts of extreme heat was delivered to doctors, nurses and paramedics at emergency departments in Karachi and, in parallel, awareness-raising activities at community level aimed to improve understanding of heat-related illnesses to reduce sickness and death.
Four major hospitals and 16 communities impacted by heat waves were surveyed to understand the changes in knowledge, behaviour and care seeking resulting from the intervention.
What were some of the key findings?
- Trust in community health workers and other non-governmental organisations increased.
- People exposed to community interventions had fewer heat-related outcomes (death, hospital visits and hospital admissions).
- Emergency physicians significantly improved their knowledge of diagnosis and management of heat-related illnesses after the intervention.
To provide a resource that could be used long-term, the study team produced a manual for healthcare professionals, with guidance on the assessment and management of patients with heat exhaustion and heat stroke. For more information you can read the study profile or this research snapshot about the outcomes and implications of this study.
How can cities best prepare for disasters?
‘Measuring Urban Capacity for Humanitarian Crisis: Piloting an Urban Health Response’. Study team: Johns Hopkins University School of Medicine; ICRC; APPNA Public Health Institute; Universidad de Fortaleza; University of Port Harcourt.
A rapid increase in urbanisation and extreme weather has exacerbated the threat of disasters and emergencies in cities around the world. Preparation and planning, to make sure that health and emergency response systems are ready to deliver life-saving care, is vital. However, few tools are available for cities to assess their emergency medical response plans.
One R2HC study sought to fill this gap, by creating a tool that would empower urban authorities to improve health response after disasters. They developed the tool CAMERA — City All Hazard Mass Casualty Emergency Response and Action. CAMERA can be used to objectively score the lifesaving capability of urban health systems, in the aftermath of a mass casualty event.
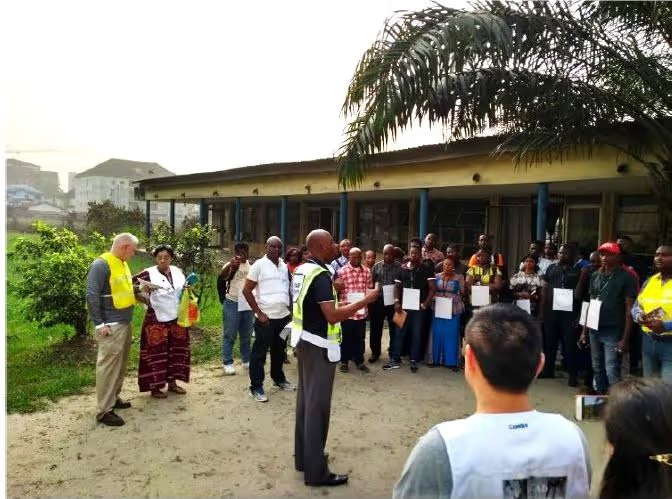
This novel tool assesses environmental, political, economic, and social factors in urban areas to reveal ways that cities could improve urban disaster response. It was tested in three low-middle income cities: Karachi (Pakistan), Fortaleza (Brazil), and Port Harcourt (Nigeria), to predict how well city authorities could respond to a disaster.
What were some of the key findings?
- CAMERA can be a reliable and valid tool to identify gaps in a city’s medical response system.
- Gaps identified by CAMERA can enable recommendations to policymakers, which will allow for frameworks and management structures to be improved for better coordination of emergency response.
In their study profile they provide an overview of the study, and their research snapshot gives more insight into key findings and outcomes. Feel free to get in touch with the team if you are interested in testing this tool.

From firewood to cleaner fuel: weighing the environmental and human health costs for Rohingya refugees
‘Human and environmental health costs and benefits of firewood versus clean fossil fuel use by Forcibly Displaced Myanmar Nationals and host communities in Bangladesh’. Study team: Stanford University; International Centre for Diarrheal Disease Research, Bangladesh; International Organization for Migration (IOM); United Nations High Commission for Refugees (UNHCR); and the Energy and Environment Technical Working Group in Cox’s Bazar.
In Cox’s Bazar, Bangladesh, Rohingya refugees depend on firewood for cooking. The daily burning of firewood by over one million refugees in the camp has led to deforestation in the surrounding area. The use of firewood for cooking indoors also presents a health hazard, leading to respiratory diseases.
This research aims to find out how distributing liquid propane gas (LPG) in Rohingya refugee camps can address the environmental and health costs of firewood. It will look at how a switch to cleaner fuel could improve a number of interlinked issues for Rohingya refugees, including food security and household income; incidences of sexual, physical, and verbal harassment and violence associated with collection of firewood; fuel expenditure; and time collecting wood and cooking.
What are the expected outcomes?
The study team hopes to add to the limited evidence base on the adoption and implementation of an LPG delivery system in humanitarian contexts. The research findings will be used to help inform the continuation of distributing LPG gas in Cox’s Bazar, in Bangladesh.
Cost-benefit models created from this study could potentially be adapted to humanitarian settings in other parts of the world, improving the health outcomes for other populations who experience negative health outcomes due to the inhalation of firewood smoke.
This study is completing data collection and analysis, with final results anticipated later in the year. Their study profile and a blog post details more about the project.
Stay updated
Sign up for our newsletter to receive regular updates on resources, news, and insights like this. Don’t miss out on important information that can help you stay informed and engaged.
Explore Elrha
Learn more about our mission, the organisations we support, and the resources we provide to drive research and innovation in humanitarian response.